What dementia treatment could mean for me: Three people living with dementia share their story
Since 2021, the U.S. Food and Drug Administration (FDA) has approved two new treatments for Alzheimer’s and dementia, Aducanumab (Aduhelm™) and Lecanemab (Leqembi™), that slows progression. While these treatments work differently, they both target beta-amyloid, a protein that forms in the brain and makes plaques. Beta-amyloid is one of the underlying causes of dementia.
In April 2022, the Centers for Medicare & Medicaid Services (CMS) issued an unprecedented decision to not cover FDA-approved treatments that target amyloid for Alzheimer’s disease, like aducanumab and lecanemab, unless the person is enrolled in an approved clinical trial. Many private insurers have followed this example.
This decision prevents people who could benefit from treatments today from receiving them even if their doctor prescribes them.
We spoke with three people who are currently living in the early stages of dementia. They share what their life was like before the disease and what having access to the treatment could mean for them.
Angela
Early retirement
Angela, who was born in Germany, moved to the United States as a young adult. She spent her first years as a waitress and portrait photographer before she began to work as office manager for small computer sales and installation companies for about 20 years. Her last position was manager of the Accounts Payable department in a large law firm.
During the end of her career with that office, she kept making more and more mistakes. “My supervisor noticed that I kept forgetting and missing important details,” said Angela. “I realized the seriousness and impact of my mistakes and therefore took early retirement.”
Angela was diagnosed with dementia at age 64.
A fantastic life
Before dementia, Angela had season tickets to the symphony and opera and would jump on the Bay Area Rapid Transit (BART) to get places. She enjoyed talking to people at the stores, the farmer’s market and engaging in lengthy discussions with librarians.
While she can still do many of these things it takes more effort for her. “I’m still doing things, but it takes more and more effort. I haven’t been in a political discussion in years. I had an extremely fantastic life and I really miss it.”
Fighting for treatment
Angela does have access to one Medicare approved medication. However, it is only treating her symptoms and not slowing the progression of the disease like aducanumab and lecanemab. “I’m fighting for the new treatment,” said Angela. “I’m outspoken about getting Aduhelm approved by Medicare. Just being mentally alert would be great. It happens a lot during conversations with friends or neighbors that I don’t have comments or the answers to their questions until I remember them hours later.
“I have been taking [a prescribed cholinesterase inhibitor] for about five years, it may have helped to slow down the worsening of my condition. But it is NOT enough! These days I often feel that my brain is failing me. I cannot concentrate on anything, forget many details and feel insecure about many things. It is getting worse and worse with every year.”
Waking up her brain
For now, Angela plans to get into better shape and travel with her partner Stewart as much as possible. “I’m going to travel as much as I can as long as I can,” said Angela. “When I get out of my usual surroundings it feels like my brain wakes up and I am so happy. That’s why I love to travel with my partner Stewart: last year we went to Hawaii and Alaska. It was fantastic and my brain was wide awake: I loved every second of it.”
Leah
Dotting her i’s
Leah spent her professional career as a therapist who also had a side specialty in corporate consulting. When she wasn’t working she was volunteering at a hospice, singing at people’s bedsides.
Leah began to notice, especially in corporate consulting, that she wasn’t as accurate as she used to be. She assumed it was just part of getting older and decided it was time to retire from consulting. “[In my work] you have to dot your i’s and cross your t’s,” said Leah. “I assumed the loosey goosey was due to cognitive decline of aging. I stopped doing corporate consulting and continued as a therapist.”
Living with MCI
Fifteen years after retiring from her career as a therapist, around the time the COVID-19 pandemic began, Leah found out she had Mild Cognitive Impairment (MCI). “My life changed because of MCI,” said Leah. “The issue with MCI is that we can’t know if it is going to get worse. Not everyone with MCI inevitably goes on to develop dementia. Some people plateau.
“The challenge for anyone living with MCI is how to live with uncertainty. If we can’t, we are apt to either stay in denial, or constantly worry and catastrophize. Initially I was terrified, but I’m gradually getting used to a ‘wait and see’ life. I worry less than I did at first, and it makes me feel grateful for what is going well.”
Better treatments
At this time, Leah doesn’t see the new Alzheimer’s treatments as a part of her treatment plan. However, she understands the importance to have those treatments available for others who are interested in them. “The issue of access to Medicare coverage is an important social situation,” said Leah. “Even though I am currently in a ‘wait and see’ holding pattern, the time may come when it will be important for me. As someone with MCI, I look forward to better treatments with fewer risks in the future and I believe it’s important for Medicare to cover [these new treatments].”
Busy all day
Since her diagnosis, Leah has volunteered on clinical trials, participates in water aerobics, joined a support group, is writing a book and currently working on writing a song about MCI. “I’m busy all day,” said Leah. “I’m working with a singer songwriter to make a really funny song about MCI. It’s going to be a great deal of fun. I also have weekly visits with my two grandsons.”
Since her initial interview, Leah finished the song she was working on. Click the play button below.
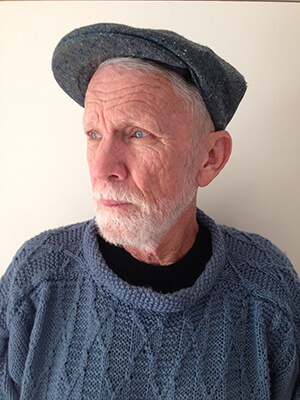
Michael
Trip to the emergency hospital
Michael, like so many other people, spent the day on January 6, 2021, watching the riots on the United States Capitol. “I got up the next morning and was out of it,” said Michael. “I kept repeating the same things over again. My wife took me to the emergency hospital where they told me I had dementia.”
After this surprising diagnosis, Michael quit driving and found his depression has gotten worse. However, what he’s most afraid of is losing his memory. “I can tell the changes over the last few months, I’m losing some of my memory,” said Michael. “That’s a big issue for me.”
Changing his future
Having access to one of the treatments would change Michael’s future, “It would change my life, outlook and plans. It would be great if it happens, but I don’t expect it to. I like to travel, we’re doing a little but I’m not sure how much longer I’ll be able to do that.
“I’ve got kids and grandkids that are a major part of my life. How do I address [the disease] especially with little kids? Even with my adult children, it’s dicey. I don’t want to make it any worse for them.”
Affording treatment
[The CMS decision] is a terrible situation. There are a few people who have enough money to buy those treatment and most of the rest of people don’t. [My wife and I are] retired teachers, we’re doing fine. There’s no way we could [pay for the treatment]. There are so many people who live on retirement who have much less than we do.”
Staying involved
Currently, Michael attends a support group specifically designed for people living in the early stages of dementia. He also writes poetry which he reads to both his support group and the Rotary club he’s still a member of. “There’s a lot of work to be done in the community,” said Michael. “It’s important to me to go [to Rotary]. Sometimes I don’t know if I’ll be able to make the effort, but I always feel better afterwards. I am far more aware of what’s going on in my life and how lucky I am to have a wife like I do who is so loving and supportive.”
Poem wet strings of beta- myloid mixed with spaghetti-like lumps attack cognitive functions and social inter-actions. but we watch for grace still briefly bestowed in brilliant landscapes windows of light insights into loving relationships that sustain usMichael
If you’re interested in helping the Alzheimer’s Association show CMS that we mean business, join us on May 24, 2023 in San Francisco. Gather with hundreds of advocates from across the state to speak up with one voice and demand #AccessNow! To participate in our Rally for Access please register here.