Loving husband of 50 years navigates wife’s younger-onset dementia
David Gunter was the primary caregiver for his wife Peggy, who was diagnosed at 57 with younger onset dementia. Because of her young age, Peggy’s dementia symptoms were dismissed as anxiety. David shares their story of getting a diagnosis for his wife, participating in clinical trials and the help and support he received after connecting with the Alzheimer’s Association®.
Meeting his wife
David and his wife Peggy technically met when she was in the 7th grade and he was a part time janitor for her middle school. David, who was five years older than Peggy, had just been drafted to the Vietnam War and was waiting for induction when Peggy decided to “accidentally” spill her milk so David would have to come to her table to clean it up. David said, “I don’t remember the event, but her girlfriend told me all about it at the class reunion.”
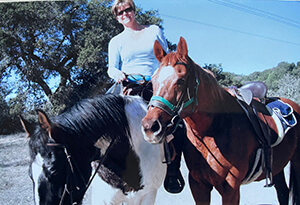
For the next three years, Peggy kept track of David through her mother who was part of a group of women putting together gift packages for servicemen overseas. When David returned home, his best friend was dating Peggy’s older sister. Peggy traded a pair of sunglasses for her sister to introduce her to David and from then on, the couple were inseparable.
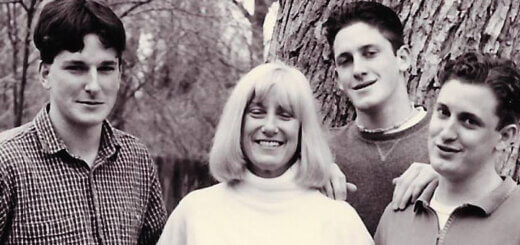
The couple married in 1974 and spent their time taking short trips while Peggy finished college and began student teaching. Five years later, the couple had the first of three boys. It was then that Peggy decided to put her career on hold until her children were older.
When her youngest started first grade, Peggy finished earning her credentials and began her 15-year career as an elementary school teacher, teaching both second and fourth grade. There she became one of the teachers that every parent wanted their kid to have.
Becoming more forgetful
When Peggy moved from teaching second grade to teaching fourth, she noticed she was becoming more forgetful, misplacing her glasses and car keys. David put up several whiteboards in their house where Peggy could put notes to remind herself to pick things up or take things to class.
David could see Peggy was struggling at her work. “I knew she was forgetful when planning the next day’s class,” said David. “I’d leave work early, help her lay out [the next day’s lesson plan] so she wouldn’t forget or lose the placement of it. She was still capable of planning for the next day, but she’d place it some place and forget where it was.”
In 2011, the school announced that due to declining enrollment they were offering teachers an early retirement package. David encouraged Peggy to take it, saying they would retire together. Reluctantly, Peggy accepted the offer and retired. “I presented [the retirement in] a fashion that I was going to retire too,” said David. “Everything we’d done up to that point, we’d done together as a team. As the school started the next year, and she saw the bus go by picking up kids, she cried. She really missed it. That was her thing in life, teaching, those were her kids in the classroom.”
A misdiagnosis
Prior to her retirement, Peggy’s problems with her memory had been bothering her, so she went to her doctor for help. Because of her young age, Peggy’s doctor assumed Peggy’s forgetfulness was just anxiety. She started to see a therapist who tried to help her cope with the anxiety. However, over time it became clear to Peggy’s family that this was more than anxiety.
Since health care providers generally don’t look for Alzheimer’s disease in younger people, getting an accurate diagnosis of younger-onset Alzheimer’s can be a long and frustrating process. Age or medical history can cause doctors to overlook or rule out Alzheimer’s disease. It’s also not uncommon to be told your symptoms may be related to stress, menopause or depression. This can lead to misdiagnosis (sometimes multiple times) and incorrect treatment.
David received an email from Peggy’s siblings telling him that Peggy didn’t need therapy; this was more than that. David said, “That [email] opened my eyes.” He took Peggy back to her doctor, who sent her to see a psychiatrist. It was only then, when Peggy couldn’t fill out the questionnaire, that the psychiatrist put the pieces together. After some additional testing, Peggy was diagnosed with younger-onset dementia at the age of 57.
Joining a clinical trial
The couple decided to be proactive and, in 2014, signed Peggy up to be part of a clinical trial. Clinical trials are research studies conducted with human volunteers to determine whether treatments are safe and effective. Without clinical research and the help of participants, there can be no treatments, prevention or cure for Alzheimer’s disease.
When David asked Peggy’s doctor which trial to participate in, they were encouraged to pick anyone as they would all be educational. Peggy enrolled in a drug trial that was intended to reduce the amount of tau (tangles) in her brain. When the study ended, 15 months later, disappointingly it was found that the drug did not work.
In 2016, Peggy signed up for another study around communication and memory loss. However, after the first day it became clear to the people running the study that Peggy’s Alzheimer’s had progressed beyond what they were looking for in a candidate and asked her to leave.
“There is a benefit to clinical trials,” said David. “You’re doing it for your own benefit but you’re [also] doing it for the benefit of those who come behind us. There are different kinds of Alzheimer’s and because [Peggy] was diagnosed with younger onset, it’s more typically an inherited gene that activates. [We did this] for our kids and grandkids. If you don’t look for a solution, you’re not going to find one.”
Finding support
Peggy’s doctor also encouraged them to reach out to the Alzheimer’s Association for help and support. There they discovered the early-stage support group. This support group is two groups running concurrently, one for the care partner and one for the person living with the disease. This type of support group gives both people the opportunity to openly share what they are personally going through.
The Association holds virtual and in-person local support groups and works to bring care and support to every community so that no one has to face dementia alone. Support groups create a safe, confidential and supportive environment. They offer participants an opportunity to develop mutual support and social relationships.
“They had group meetings once a month,” said David. “It was a discussion on what you were going through. [The support group helps you] feel that you’re not alone. Many of us are going through the same thing. Maybe in a different way but the same struggles.”
Prepare for the future
David encourages new caregivers to prepare for the future as best they can, especially when it comes to finances. “First thing we did was to put our assets in order,” said David. “We opened a trust. We may not have much but we had a home. I put those in a trust [so my kids don’t have to] sit and wait for a probate judge to say who gets what.”
Sadly, Peggy died in September of 2024; three months short of their 50th wedding anniversary. David cared for her in their home until the end. “Things change and it changes quickly. When I look back on our life together, we had 50 years together. I really feel fortunate. Other couples don’t get that.”
For more information on Alzheimer’s support groups visit alz.org/norcal/support. If you’re interested in signing up for a clinical trial visit alz.org/trialmatch.