Roseville woman’s story about stress and finances in dementia care
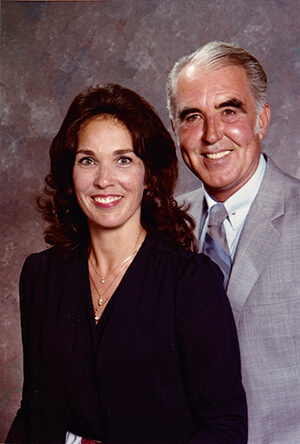
Noriene Butterfield spent nearly a decade caring for her husband Tom, who had dementia with Lewy bodies. During this time, she faced emotional and financial challenges, continuing to work despite being of retirement age, to cover Tom’s care. The stress of working and being a full-time caregiver led Noriene to experiencing panic attacks. Noriene shares how the Alzheimer’s Association® support groups helped her cope and how she continues to help other caregivers.
Getting the job done
Tom Butterfield began working as a crane operator in the early 1950s. He dedicated his life to his team and his company, always the guy that got the job done when no one else could. He worked his way up until he became an operating engineer’s union official. Tom retired in the 1990s at the age of 60.
“When he was married to his second wife, they had a party at their house one night,” said Noriene. “Everyone from work was there. [The company called and asked if someone could come in], guess who worked, Tom. Another time, he and his wife were supposed to be on vacation, [work called]. Tom said, ‘That old man needs me. He keeps me busy in the winter, he needs me, I’m here.’ That’s the kind of a person Tom was as a worker.”
In addition to caring for his four children, Tom was the kind of guy that went to hang out with old coworkers who had retired. He’d call and check on them or would stop by to sit and have a beer. Noriene said, “He was a friend. He wouldn’t golf or bowl, but he’d sit and drink a beer with you.”
Self-isolation
While it is important to take steps to care for your brain your whole life, it is especially important when you retire. Positive, routine actions can make a difference in brain health, even lowering the risk of cognitive decline and possibly Alzheimer’s disease and dementia. Science suggests that lifestyle habits that improve your overall health, such as exercising, consuming a nutritious diet — and staying cognitively and socially active may support brain health.
After Tom retired, he began to self-isolate, staying home, reading the paper, watching tv and only going out to walk his dog, Abigail. Noriene did her best to try to get him to learn new things, join the senior center or travel. Noriene, who was several years younger than Tom, went so far as to retire early so they could see the world together. But after a few years with only three short trips in the books, Noriene decided she wanted to go back to work and school.
It was in her last semester of college in 2005 that Tom’s behavior noticeably began to change. He got angry that Noriene was still in school, despite Noriene having attended numerous classes in the past with no issues from Tom. When Noriene took a solo trip to China, she got sick and Tom had little sympathy for her and told her to just stay there until she was better, something completely out of character for him.
Noriene had brought Tom’s odd behaviors to the rest of the family, but because the kids didn’t see Tom acting any differently, they didn’t believe her. Whenever the kids were around, Tom was able to act like everything was fine. It wasn’t until 2010, when Tom told everyone that his long-deceased father called and asked Tom to bring him a gun, that the kids finally saw what was happening.
“We’re at the house and the kids were there,” said Noriene. “[Tom] said, ‘Pop called and wanted me to bring him a gun.’ [Tom’s] dad died in 1992. I said, ‘Well Liz, [Tom’s niece], has your dad’s ashes.’ [Tom called Liz] and after talking to Tom, she called me and said, ‘I thought he was kidding, but he’s as serious as a heart attack.’ Then the kids started realizing what was wrong.”
Hallucinations
Noriene was able to get Tom in to see a neurologist who diagnosed him with Alzheimer’s and later dementia with Lewy bodies (DLB).
DLB is a type of progressive dementia that leads to a decline in thinking, reasoning and independent function. Its features may include spontaneous changes in attention and alertness, REM sleep behavior disorder, and slow movement, tremors or rigidity, and even recurrent visual hallucinations
Tom was convinced that someone from work came to his house with over $160,000 in cash, and because it was such a large amount, they were going to put it in a bank for him. Tom had his son drive him all over town looking for it. Another time, Tom called the police because Noriene’s work had sent him somewhere and he believed they beat him up and took his money, but Tom hadn’t left the house that day.
Panic attacks
Tom’s hallucinations continued throughout the rest of his life and understandably added to the stress of caring for someone with dementia. According to the Alzheimer’s Association Alzheimer’s Disease 2024 Facts and Figures report, 59% of caregivers of people with dementia rated their emotional stress of caregiving as high or very high. Spousal caregivers are more likely to experience increased burden over time.
As a person with dementia’s symptoms worsen, caregivers can experience increased emotional stress and depression; new or exacerbated health problems; and depleted income and finances. The report shares that dementia caregivers in the United States are 26% more likely to experience anxiety and that the prevalence of anxiety is 44%.
Caring for Tom took a toll on both Noriene’s physical and mental health. Every day Tom would come to her and tell her that it was time for him to go home to his wife, and Noriene would cry. She started having severe panic attacks, something she’d never experienced before. She also threw out her back. The doctors told her she’d need her spine fused which caused her to be in a wheelchair and a walker for some time.
“People don’t realize the caregiver is the one that really goes down,” said Noriene. [A friend of mine’s] wife has dementia. He just had a heart attack and died. He was doing it all himself, and you can’t do it all yourself.”
Moving to a care setting
Eventually, there came a time when Tom needed his hip replaced. Noriene has been putting it off for years, knowing that the anesthesia could cause Tom’s symptoms to increase more rapidly. Worried for both her and Tom’s safety, Noriene spoke with the kids and decided that after the surgery, Tom would need to move into a care setting.
Noriene found a nearby place that would allow Tom to bring his own things like photos and furniture to use while he lived there. He continued to remain at the care setting after his surgery until a few years later when he fell, and he had to be moved to someplace that offered 24/7 care. Tom lived there until his death in 2014.
The cost of care
The Facts and Figures report states that six in 10 dementia caregivers were both providing care while simultaneously working. Nine percent of caregivers had to give up work entirely and an additional 6% retired early.
Data from the 2016 Alzheimer’s Association Family Impact of Alzheimer’s Survey indicated that 48% cut back on other spending and 43% cut back on savings due to the out-of-pocket costs of providing help to someone with dementia.
Tom’s care costs, especially after moving into the care setting, were $7,000 to 8,000 a month. Because of the high costs, Noriene could not afford to retire. Despite working full time, and Tom’s pension from the Union, there still wasn’t enough money to cover both her cost of living and Tom’s care. This forced Noriene to start claiming her social security benefits earlier than she would have liked, reducing the amount of money she could have potentially received had she waited until she was older.
Over the course of the disease, Noriene spent more than $350,000 on Tom’s care. She continued to work for an additional three years in order to save enough money to live on after she retired. If it weren’t for Tom’s pension, Noriene may still be working now.
Finding much-needed support
While Tom was still alive, Noriene found the Alzheimer’s Association. There she was connected to a support group where she found like-minded people going through a similar experience as she was. “The Alzheimer’s support group was a life saver for me,” said Noriene. “If you can get time to go to the support group, go. Not only were they going through it at the time, people who had lost their spouses were still coming [back] to help us.”
Noriene also began attending the Alzheimer’s Association Walk to End Alzheimer’s® in the hopes of finding a cure. Since Tom’s initial diagnosis, Noriene has moved around a few times and has attended the closest Walk to her. This includes both ones in Northern Nevada and Northern California such as in the East Bay, and Solano County. This year her closest Walk will be held in Sacramento.
Resources
Through her time at the support group, Noriene discovered a book called, “The 36-Hour Day,” which she recommends to everyone. “There are so many things, people don’t understand,” said Noriene. “’The 36-Hour Day’ book was my bible. We read the chapter with whatever Tom was going through at the time. I have bought that book for so many people. I have tried to help so many people who are going through this situation.”
The other piece of advice Noriene gives to people is to reach out to the Alzheimer’s Association 24/7 Helpline (800.272.3900). The 24/7 Helpline is a free service offering support for people living with dementia, caregivers, families and the public. There you will connect with a live person who can provide information, local resources, crisis assistance and emotional support. Noriene said, “If you need to talk to someone any time, someone is there to talk to you.”
Noriene encourages other caregivers to reach out to the Association for support and education. Her hope is that one day, there will be a cure. On the night of Tom’s death, his granddaughter Marisa climbed in bed with him and for a moment he knew who she was and called her by her name. Noriene says, “The bright light for me is that [he wasn’t alone], he was with Marisa, the night he died. That helped heal my heart.”
You can find more information on caregiver stress at alz.org/caregiverstress. Put your legal and financial plans in place today, learn more about financial and legal planning on our website.
Join a caregiver support group near you, visit our event page to find a support group near you.