Legislators Hear the Needs of Nevada Caregivers
Volunteers advocate for improved services for those living with Alzheimer’s.
What would you do if you were the sole caregiver for a parent with dementia and you needed surgery? Who would take care of your parent during your recovery if you didn’t have funds to pay for caregivers?
This is the dilemma facing Susan, of Carson City, Nevada. She puts her own health needs aside to care for her mother, who has vascular dementia.
Sharing her story with legislators
Susan recently shared her story at a listening session on the behavioral and cognitive needs of older adults in Nevada. Current and former caregivers from across the state shared challenges they have faced.
Speaking before a legislative committee can be intimidating. The caregivers who bravely shared their stories (oral or written) will help shape the availability of services.
Highlights from the listening session
Legislators express concern for older Nevadans
Last year, the Nevada Legislature passed Senate Bill 121. This law calls for a legislative committee to study the behavioral and cognitive care needs of Nevada’s aging population.
The committee is chaired by Senator Joyce Woodhouse, who authored S.B. 121. Members have been seeking input from stakeholders throughout Nevada. They want to learn about the challenges caregivers face and the needs of older adults.
A growing burden on caregivers
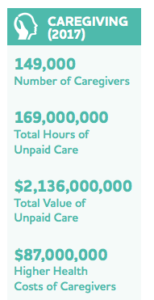
More than 45,000 Nevadans currently live with Alzheimer’s disease. That number is predicted to grow to 64,000 by 2025, the third highest increase of all 50 states. There is an urgent need to develop solutions to the current challenges.
In Nevada, more than half of unpaid caregivers of those with Alzheimer’s or another dementia have been providing care for at least two years (Centers for Disease Control and Prevention; 2016 Behavioral Risk Factor Surveillance System). Nearly 40 percent provide 20 or more hours of care per week.
Many are managing very personal tasks:
- 80.9 percent manage household care, such as cleaning or cooking.
- 59.6 percent manage personal care, such as feeding or bathing.
The challenge of providing personal care
Patti, from Winnemucca, is one of those individuals providing personal care. Patti cares for Harold, her husband of 45 years, who is in the late stage of Alzheimer’s.
Harold is very aggressive and doesn’t like to be touched. He is also afraid of using the toilet. His reaction to being touched and fear of using the toilet makes it difficult for Patti to provide bathroom-related care without getting injured.
Harold is a veteran and has received services from the Veterans Administration (VA). The closest care facility that the VA will cover is in Henderson, a 12-hour drive. There is a memory care facility near Patti, but the VA will not pay for care at that facility and Patti cannot afford it on her own.
Listening to caregivers statewide
The Alzheimer’s Association hosted the statewide listening session in March. We partnered with the Aging and Disability Services Division and the Division of Public and Behavioral Health. Family and professional caregivers from six Nevada communities shared their experiences.
Over 100 individuals from six locations took part in the session, with many providing oral or written testimony. Caregivers discussed the barriers they faced. They also offered suggestions for supporting the care needs of those living with dementia.
Common challenges
Recently, the Alzheimer’s Impact Movement (AIM) conducted a nationwide poll. When compared to other major diseases like cancer and heart disease, voters believe Alzheimer’s poses the greatest risk to their retirement.
Nevada’s communities vary widely from more densely populated Clark and Washoe Counties to sparsely inhabited rural and frontier communities. It was clear that while many Nevada caregivers feel alone and isolated, they are part of a growing caregiving community.
The most pressing needs identified fall into five categories:
- Shortage of respite – caregivers in every community expressed the need for reliable, quality respite care to provide relief for family caregivers.
- Insufficient awareness and education – even where resources existed, care providers were not always aware of or able to access them.
- Perceived lack of dementia-competency training – providers (medical, respite, and long-term care) and families requested more or expanded training.
- Limited availability of affordable long-term care and staff to provide care – it is difficult to find and access long-term care at reasonable rates. Also, there are limited incentives for providers to work in rural areas, so it can be impossible to hire in-home care or staff existing facilities adequately.
- Inadequate availability of affordable transportation – transportation issues create a barrier to accessing and safely use services, which can increase isolation.
Waiting up to two hours for a ride
Paul of Las Vegas has been caring for his wife, Dixie, since she was diagnosed with Alzheimer’s in 2014. Dixie attends the Adult Day Care Center of Henderson six days a week. Paul can afford it because of a grant he received from Nevada Senior Services.
Paul uses Paratransit to get Dixie to and from the adult day center, but there’s a two-hour window for pickup in each direction. Paul must have Dixie ready and waiting with him for up to two hours at the pickup site – regardless of weather. He must also wait there for up to two hours for Dixie to be dropped off.
Recommendations for the committee
Those in a caregiving role (family caregivers or professionals) should have the information, tools and resources they need to provide quality care. This kind of care preserves autonomy for individuals with dementia, can help avoid institutional placement and improves quality of life.
In reviewing findings from the listening session, we made three recommendations to the committee:
- Expand respite – through enhanced/alternate funding sources, increase ease of access to respite resources; bolster programs that recruit and train respite volunteers statewide.
- Increase public awareness of services – promote use of existing services through a coordinated, statewide public awareness campaign.
- Review training and education requirements for providers – review Nevada statutes & codes for consistency in dementia training requirements amongst all facilities and health professionals.
Committee’s next steps
The committee has been gathering data from a variety of sources within the state. Members have also heard testimony from programs in other states, as they seek best practices.
After their final meeting in June, the committee will make recommendations, which may include new legislation, budget requests and/or changes in statute/code. They will submit their findings and recommendations for the 2019 legislative session.
We have been impressed by the efforts of the committee. “Clearly they are committed to making recommendations that will have lasting impact on people with Alzheimer’s and other dementia in Nevada, including the rural communities,” stated Ruth Gay, Chief Policy Officer of the Alzheimer’s Association, Northern California and Northern Nevada Chapter. “We look forward to supporting the implementation of their recommendations.”
If you are living with Alzheimer’s or another form or dementia or are a caregiver, please call 800.272.3900 or visit our website to learn about resources available to support you. Learn more about sharing your story to improve policies related to Alzheimer’s.
Learn More:
- Nevada Interim Committee to Study the Needs Related to Behavioral and Cognitive Care of Older Persons
- National and Nevada Alzheimer’s Facts and Figures
- Data on Dementia Caregiving in Nevada, Behavioral Risk Factor Surveillance System
- Caregiver support
- Find community resources (nationwide)
- Become an advocate
- Share what you have learned