Palliative Care and Hospice Education and Training Act (PCHETA)
Observational studies have shown that as many as half of nursing home residents with advanced dementia have documented pain in the last weeks of life – and about a third have difficulty breathing and swallowing, or suffer from agitation.
Individuals with advanced dementia who are enrolled in hospice have a lower rate of dying in the hospital, a lower rate of hospitalization in the last 30 days of life, and better symptom management.
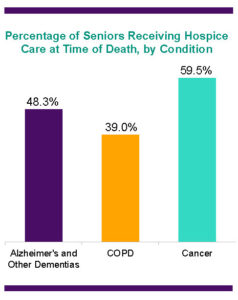 Recent studies show that nearly half of all people with Alzheimer’s and other dementias are in hospice care at the time of their death. However, the current availability and quality of palliative and hospice care is a concern.
Recent studies show that nearly half of all people with Alzheimer’s and other dementias are in hospice care at the time of their death. However, the current availability and quality of palliative and hospice care is a concern.
Palliative care focuses on managing and easing symptoms, reducing pain and stress, and increasing comfort. Less than half of surveyed nursing homes report having some sort of palliative care program. Of those nursing homes with a palliative care program, only 42 percent include consultation by a physician certified in hospice/palliative care, and only 28 percent had a designated director of palliative care.
For people with advanced dementia, such care improves quality of life, controls costs, and enhances patient and family satisfaction.
As the demand for palliative services grows with the aging population in the United States, more must be done to ensure an adequately trained workforce. That is why the Alzheimer’s Association strongly supports the bipartisan Palliative Care and Hospice Education and Training Act (PCHETA), which was introduced by Representative Eliot Engel (D-NY-16) and Representative Tom Reed (R-NY-23) in the U.S. House of Representatives and Senator Tammy Baldwin (D-WI) in the U.S. Senate.
The Palliative Care and Hospice Education and Training Act (S. 2748/H.R. 3119) would increase palliative care and hospice training for health care professionals, and inform patients and their families about its benefits.
A recent study shows that nursing home residents with dementia who receive palliative care at the end of life, compared with those who do not receive such care, are:
- up to 15 times less likely to die in a hospital
- nearly 2.5 times less likely to have a hospitalization in the last 30 days of life
- up to 4.6 times less likely to have an emergency room visit in the last week of life.
People with Alzheimer’s and other dementias rely heavily on hospice at the end of life.
- Of all people living with dementia, 18.6 percent receive hospice care in a given year – a higher percentage than other chronic conditions.
- Among seniors in hospice care, one in every five has a primary hospice diagnosis of Alzheimer’s or other dementia.
- Nearly half of all people with dementia die in hospice care.
The availability of palliative and hospice care is growing, but the need is growing faster – and the quality of the care remains a concern. In the 2014-15 academic year, only 265 physicians were trained in hospice and palliative medicine by accredited programs. An expert Task Force concluded that 6,000 more full-time health care professionals are needed to serve current needs in hospice and palliative care programs.
To increase the availability and quality of care, PCHETA would establish palliative care and hospice workforce training programs for doctors, nurses, and other health professionals. It would also create a national education and awareness campaign to inform patients, families, and health professionals about the benefits of palliative care and available services and supports. Finally, it would enhance research on improving the delivery of palliative care across the country. Watch the below video to learn more.
https://www.youtube.com/watch?v=ku31jfOH_4k
Helpful information related to this post:

















Completely agree with you, patients suffering from Alzheimer, dementia are better handled and managed through the hospice care or hospitals with the fully equipped palliative care facility, which is more humane, comfortable, compassionate and eases the pain.