Alzheimer’s and Dementia Testing for Earlier Diagnosis
 What if we could diagnose Alzheimer’s before symptoms started? The hope is, future treatments could then target the disease in its earliest stages, before irreversible brain damage or mental decline has occurred. Research on new strategies for earlier diagnosis is among the most active areas in Alzheimer’s science, and funding from the Alzheimer’s Association has spurred significant advances and steady progress.
What if we could diagnose Alzheimer’s before symptoms started? The hope is, future treatments could then target the disease in its earliest stages, before irreversible brain damage or mental decline has occurred. Research on new strategies for earlier diagnosis is among the most active areas in Alzheimer’s science, and funding from the Alzheimer’s Association has spurred significant advances and steady progress.
Biomarkers for earlier detection
Experts believe that biomarkers (short for “biological markers”) offer one of the most promising paths. A biomarker is something that can be measured to accurately and reliably indicate the presence of disease. An example of a biomarker is fasting blood glucose (blood sugar) level, which indicates the presence of diabetes if it is 126 mg/dL or higher.
Several potential biomarkers are being studied for their ability to indicate early stages of Alzheimer’s disease. Examples being studied include beta-amyloid and tau levels in cerebrospinal fluid and brain changes detectable by imaging. Recent research suggests that these indicators may change at different stages of the disease process.
There are currently no validated biomarkers for Alzheimer’s disease, but researchers are investigating several promising candidates, including brain imaging, proteins in cerebrospinal fluid, proteins in blood and genetic risk profiling.
Imaging technologies used in Alzheimer’s research
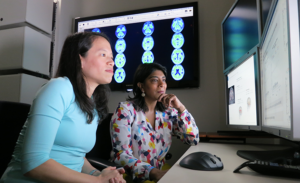 Structural imaging provides information about the shape, position or volume of brain tissue. Structural techniques include magnetic resonance imaging (MRI) and computed tomography (CT). Structural imaging studies have shown that the brains of people with Alzheimer’s shrink significantly as the disease progresses. Research has also shown that shrinkage in specific brain regions such as the hippocampus may be an early sign of Alzheimer’s.
Structural imaging provides information about the shape, position or volume of brain tissue. Structural techniques include magnetic resonance imaging (MRI) and computed tomography (CT). Structural imaging studies have shown that the brains of people with Alzheimer’s shrink significantly as the disease progresses. Research has also shown that shrinkage in specific brain regions such as the hippocampus may be an early sign of Alzheimer’s.
Functional imaging reveals how well cells in various brain regions are working by showing how actively the cells use sugar or oxygen. Functional techniques include positron emission tomography (PET) and functional MRI (fMRI). Functional imaging research suggests that those with Alzheimer’s typically have reduced brain cell activity in certain regions. For example, studies with fluorodeoxyglucose (FDG)-PET indicate that Alzheimer’s disease is often associated with reduced use of glucose (sugar) in brain areas important in memory, learning and problem solving.
Molecular imaging uses highly targeted radiotracers to detect cellular or chemical changes linked to specific diseases. Molecular imaging technologies include PET, fMRI and single photon emission computed tomography (SPECT). Molecular imaging technologies are among the most active areas of research aimed at finding new approaches to diagnose Alzheimer’s in its earliest stages. Molecular strategies may detect biological clues indicating Alzheimer’s is under way before the disease changes the brain’s structure or function, or takes an irreversible toll on memory, thinking and reasoning.
Cerebrospinal fluid (CSF) proteins
CSF is a clear fluid that bathes and cushions the brain and spinal cord. Adults have about 1 pint of CSF, which physicians can sample through a minimally invasive procedure called a lumbar puncture, or spinal tap. Research suggests that Alzheimer’s disease in early stages may cause changes in CSF levels of tau and beta-amyloid, two proteins that form abnormal brain deposits strongly linked to the disease.
Proteins in blood or other parts of the body
Researchers are also investigating whether pre-symptomatic Alzheimer’s disease causes consistent, measurable changes in urine or blood levels of tau, beta-amyloid or other biomarkers. In addition, scientists are exploring whether early Alzheimer’s leads to detectable changes elsewhere in the body. For example, Lee Goldstein, MD, PhD, has been funded by the Alzheimer’s Association to investigate whether beta-amyloid forms characteristic deposits in the lens of the eye.
Genetic risk profiling
Scientists have identified three genes with rare variations that cause Alzheimer’s and several genes that increase risk but don’t guarantee that a person will develop the disease. Investigators worldwide are working to find additional risk genes. As more effective treatments are developed, genetic profiling may become a valuable risk assessment tool for wider use.
To learn more about biomarkers and the quest for better Alzheimer’s drugs and clinical trials, watch this video from our recent Sacramento education conference.
Helpful information related to this post:

















